Other Eye
Conditions
Pterygium
A pterygium is a triangular fleshy growth that extends from the conjunctiva onto the cornea. Mild pterygia may cause dry eye symptoms such as grittiness and redness. Larger pterygia may cause astigmatism and make it difficult to fit contact lenses, or even grow across the cornea to cover the pupil and obstruct vision.
Surgery is required when vision is threatened or the pterygium is causing significant symptoms. There are a number of methods used by surgeons to remove a pterygium. Dr Forrest currently uses a technique in which the pterygium is removed and a graft taken from the conjunctiva on the eye under the patient’s upper lid is used to cover the defect left after pterygium removal. This technique is known as autologous conjunctival transplant, and is done to reduce the risk of recurrence.
With this technique the risk of recurrence is very small. The graft is sutured in place using absorbable sutures which do not have to be removed. All tissue removed is sent by Dr Forrest to a pathology practice for histological examination to ensure that there is no malignancy (cancer).

Glaucoma

Glaucoma is a disease in which the optic nerve is damaged in a characteristic way, eventually leading to loss of vision and blindness.
Timely treatment can reduce or even avoid this damage. Glaucoma affects both adults and children. In children the disease is virtually always caused by raised intraocular pressure (IOP), but not all adults with glaucoma have elevated IOP. Nevertheless reducing the pressure is the only effective treatment.
For most adult patients this is achievable with laser treatment (selective laser trabeculoplasty or SLT) or eye drops, but some patients will require surgery. In the last decade minimally invasive glaucoma surgery (MIGS) techniques have been developed, including micro-stents that can be implanted into the eye during cataract surgery.
In adults with glaucoma there are usually no symptoms until the disease has caused a lot of damage. Most patients diagnosed early are discovered to have glaucoma or be at risk of glaucoma on routine examination or after seeking assessment because of a family history of glaucoma. Dr Forrest recommends regular optometric visits, even if you have no symptoms or vision problems.
Childhood Glaucoma
Glaucoma in babies and young children is rare, and is very different from adult glaucoma. It causes symptoms of tearing and severe light sensitivity. The eye enlarges and the cornea can look large and cloudy.
Children with glaucoma invariably require surgery to lower the intra-ocular pressure and control the disease, but additionally will usually require glasses and sometimes patching to restore vision.
The most common surgical procedures are trabeculotomy and goniotomy, but other more invasive procedures may be required.

Macular Degeneration
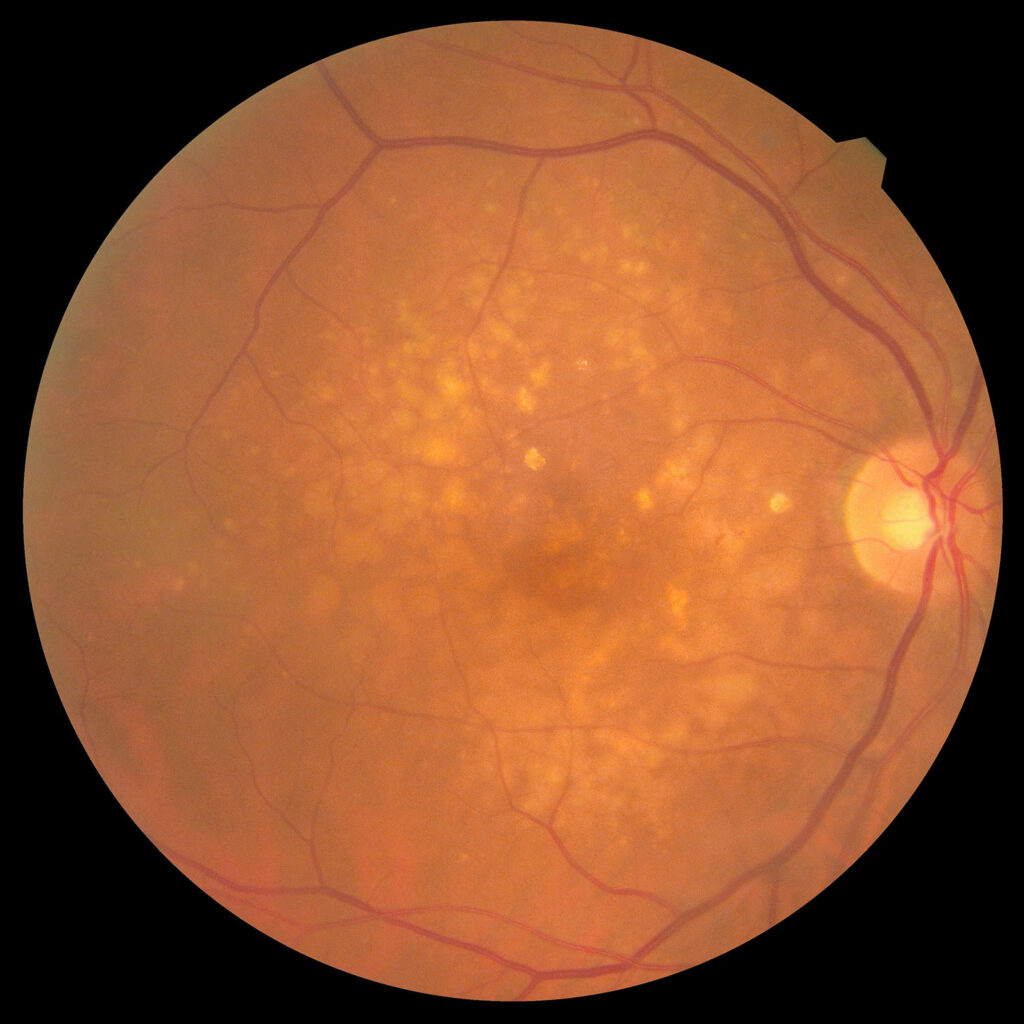
Age related macular degeneration (AMD) is a condition which affects the central part of the retina (the macula), resulting in a loss of central vision. The retina is the innermost layer of the eye, and contains the cells that respond to light (the photoreceptors) and the nerves that connect them to the brain for processing. AMD is a major cause of visual impairment in patients over 50 years old, and although peripheral vision is usually not affected, AMD can stop people from reading, driving, or recognizing faces.
The cause of AMD has not been identified, but risk factors include age, family history and smoking.
There are two main types of AMD: “dry” and “wet”. In dry AMD the retinal pigment epithelium which supports the retina thins or atrophies, and there is loss of the photoreceptors.
In wet AMD, which is usually more aggressive, growth of abnormal blood vessels leads to leakage of blood and protein that damages the macula’s photoreceptors.
Since the mid-2000s a new class of injectable drugs (anti-VEGF agents) has been proven to effectively treat many patients with wet AMD. Lucentis (Ranibizumab), Eylea (Aflibercept) and Avastin (Bevacizumab) are available in Australia, and Lucentis and Eylea are PBS-listed.
The Macular Degeneration Foundation website is an excellent source of further information about AMD, including downloadable fact-sheets translated into Italian, Greek, Chinese, Vietnamese and Arabic.
DIABETIC RETINOPATHY
Diabetic retinopathy is damage to the retina occurring as a complication of diabetes mellitus. It affects up to 80% of all patients who have had diabetes for 10 years or more, and can cause visual impairment and blindness.
Small blood vessels – like those in the eye – are most vulnerable to fluctuations in blood sugar, and are damaged by high levels of blood glucose. The vessels can leak fluid (leading to swelling or edema), or close off (leading to ischemia and tissue death in the retinal tissue these vessels supply). As damage worsens, the disease can enter a more aggressive stage with growth of new blood vessels. These new vessels are fragile and can bleed, eventually leading to tractional scarring and even retinal detachment. New blood vessels can also grow onto the iris and into the drainage angle in the front of the eye causing neovascular glaucoma, an extremely aggressive form of glaucoma.
Often there are no early signs. Swelling of the central retina, or macular edema, causes blurred vision, but if the macula is not affected quite severe diabetic retinopathy can occur without symptoms. Damage that occurs before the development of new vessels is called non-proliferative diabetic retinopathy (NPDR), and once new vessels appear it is called proliferative diabetic retinopathy (PDR).
The risk of developing diabetic retinopathy increases the longer you have diabetes, but good control can reduce that risk considerably. Cigarette smoking and high blood pressure increase risk. Because early diabetic retinopathy has no symptoms, and because treatment can be very effective at protecting vision if given early enough, regular check-ups are essential.